+7 (929) 727 53 60 Traumatology / Orthopedics / Neurosurgery
Production
1.Cleaning and material handling. Bioplant preparation Lyoplast
[gallery1]
Lyoplast products guarantee the safety of the recipient against the transmission of any disease through allogeneic tissues, which is due to the technology of cleaning and processing of Lyoplast materials.
All donors are required to conduct autopsies and serological blood tests for syphilis and hepatitis B, C and AIDS.
The Samara Bank of Fabrics uses the original algorithm for the manufacture of biological products from human tissue, protected by patents of the Russian Federation.
Selected material samples from donors undergo 6 degrees of purification mainly by physical methods (mechanical, ultrasonic, vacuum, radiation, etc.).
- At the first stage, the process of obtaining implants includes a special ultrasonic treatment of tissues for removing elements of the bone marrow and fat from the spongiosis, carrying out the primary sterilization of the material, viral inactivation.
- Only solvents for final degreasing and demineralization are used as chemical agents, and their application is extremely limited.
- The technology excludes almost 100% of traces of foreign and technological substances and solvents.
- After preprocessing, the tissues are lyophilized, and then the hermetically packed material is sterilized by radiation.
- The finished material is packaged, sterilized with gamma rays and stored at an appropriate temperature in a cool dry place.
- The production technology of bioimplants "LYOPLAST" allows the recipient to be fully protected from the transmission of any disease to him, minimizes the risk of infection to personnel and makes the process environmentally safe and economical.
Treatment of bioimplants using physical factors:
- Vacuum
- Ultrasound 26 - 40 kHz
- Lyophilization
- Gamma sterilization (fast electron sterilization).
All donors undergo autopsy and serological blood tests for syphilis and hepatitis B and C viruses, AIDS.
Serological tests are carried out to all donors before tissue sampling.
Serological testing for antibodies to pale spirochete:
- Express analysis;
- Complement binding reaction.
Serological tests for markers of viral infections:
- HBsAg;
- AntiHCV;
- Antibodies to HIV.
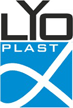
2. The surface and structure of the material for the manufacture of bioimplants
[gallery2]
Allogeneic materials from bone and other types of connective tissue, that is, alien to the recipient, but taken from a donor of the same species after their special treatment, almost completely lose their antigenicity and do not adversely affect it when placed in the body.
Here they play the role of the matrix, the conductor, and the demineralized bones, the inductor, gradually dissolve completely, and the patient’s own bone tissue forms in their place.
With a rational method of application, such bioimplants provide reparative regeneration, realizing the genetic capabilities of the organism itself - the ability of connective tissues to fully regenerate them.
Bioimplants should be manufactured in accordance with the shape, size and volume, according to the specifications:
- The surface of bioimplants should be without cracks, without break-offs and shells.
- The color of bone bioimplants should be white, gray or ivory.
- The relative content of lipids in cancellous bone tissue is (1.2 ± 1)%.
- The moisture content in bioimplants should be no more than 5%.
- Hydrogen indicator (pH) of bioimplants should be in the range of 4.0-8.0 pH.
- The dispersion of the powder should be in the range of 103-101.
- Bioimplants must be sterile.
The sterilization method is radiation. Dose of sterilization (20.0 ± 5.0) kGrey.
Individual packaging of bioimplants should be airtight.
The average shelf life of bioimplants should be 3 years.
3. Full accurate chemical composition of materials
[gallery3]
"Lyoplast-S" is the most adapted in the world in terms of its biochemical composition to the human body osteoplastic materials and membranes.
Bioimplants obtained using the "Lyoplast®" technology consist only of components of the human body and do not contain chemicals introduced from the outside.
4. Scheme of material demineralization to obtain DM-forms
[gallery4]
Within the framework of a closed cycle of waste-free production, specialists in a tissue bank simultaneously receive two types of materials: a de-mineralized bone matrix and a new material — the mineral component of human bone tissue — allogenic hydroxyapatite.
The obtained mineral-containing material, in contrast to synthetic hydroxyapatite, besides calcium and phosphorus salts, contains trace elements and glucosaminoglycans in the same proportions as they are in human bone tissue.
5. Analyzes and properties of bio-implants Lyoplast
[gallery5]
Allogeneic materials taken from a donor of the same biological type after their special treatment almost completely lose their antigenicity and do not adversely affect the organism in which they are placed.
They become a matrix (conductor), and in relation to the demineralized bone, they are also an inducer of osteogenesis.
These conductors gradually completely dissolve, and in their place a new patient's own bone tissue is formed.
In other cases, the transplant may be the carrier of osteoinductive proteins (morphogenetic proteins) that stimulate mitogenesis (division) of undifferentiated perivascular (adventitious) cells into osteoprogenital mesenchymal cells, which then turn into osteoblasts and give rise to new bone tissue.
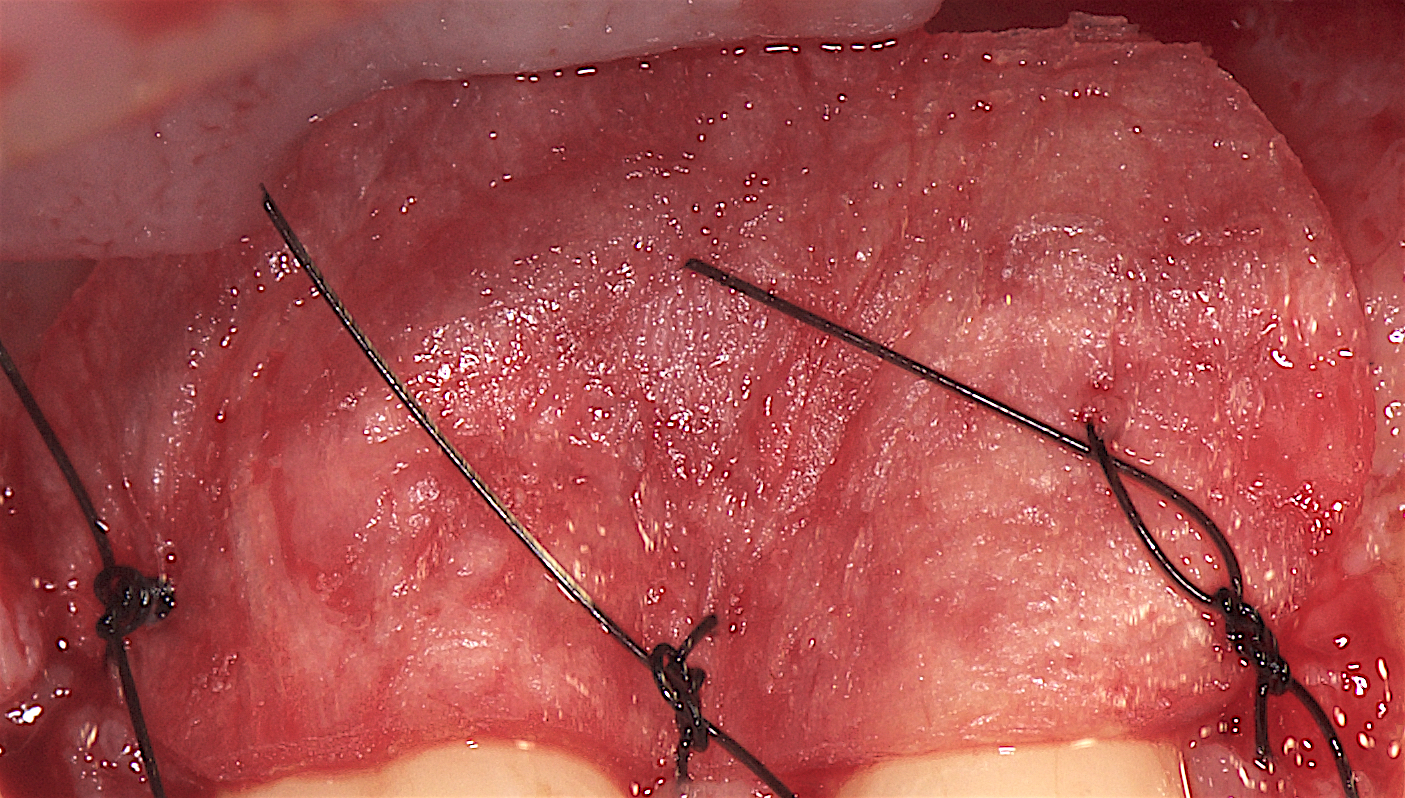
6. Full replacement of bioimplants with own body tissues
[gallery6]
The use of "Lyoplast-S" guarantees complete restoration of the patient's bone tissue in 100% of cases. Clinically proven!A wide range of standard products (powder, chips, blocks, TMO membranes) for all types of bone grafting and periodontal surgery.
The principle of differentiated selection of demineralized bone implants developed by the University, which is based on the anatomical-histological and regenerative potencies of damaged epithelial and connective tissues, ensures complete regeneration of the patient's damaged bone tissue and preservation of the anatomical integrity of the organ.
The results of surgical interventions using allogeneic bioimplants under certain conditions are not inferior to osteoplasty using the patient's own tissues.
With a rational method of application, such bioimplants provide reparative regeneration, realizing the genetic capabilities of the organism itself - the ability of connective tissues to fully regenerate them.
All materials and preparations for dentistry are completely resorbed and replaced by their own tissues.
7. Biological sense of material purification technology
Ultrasound is a destructive factor and it has a detrimental effect on biological structures.
But under certain conditions (frequency and exposure time, it can be used to remove only part of the structures, this happens at a low frequency.
This removes all traces of fat, protein, nucleic acids, dead cells and their components, non-collagen proteins and other compounds.
After this stage, only the collagen-mineral skeleton of the dead intercellular substance of bone tissue remains.
The intercellular substance of bone tissue is always dead and its composition is stable throughout the life of the bone.
During the subsequent lyophilization, all free and bound moisture flies out of the bone and it is slightly reduced in volume, as it "sits down" by 10-15%.
In this case, the so-called “capillary effect” or negative surface tension occurs in the entire volume of the porous structure.
Pressure is discharged. Therefore, the first free liquid phase in which the material will be immersed - it will actively suck for 2-3 minutes.
This hydration time is sufficient for soaking the powders.
- TMO is also soaked for 2-3 minutes or hydrated in the surgical field immediately.
- Blocks soak 3-5 minutes. It is best that this was capillary blood.
8. Briefly on the use of materials Lyoplast
[gallery7]
Mineralized spongy or cortical bone is used where it is necessary to preserve the volume in height and width, for example, in the operation of lifting the maxillary sinus or the operation of implanting teeth.
Demineralized bone is used additionally to repair internal bone defects - blood vessels grow better through it, as it contains MGB.
They are by their nature of collagen origin, therefore they are not washed out of the matrix and retain their biological properties.
Alogenic hydroxyapatite is used with an increase in volume of more than 5 mm in height.It is possible to raise the height of the sinus by 12-13-15 mm.
The ICC (Mineral Bone Component) "Lyoplast" can be used in cases of "age" patients, various disorders of mineral metabolism in the body.MCC "Lyoplast" contains: Ca, Mn, P, Fe, Zn, Co, Ag, chondroitin sulfate and collagen.
Restoration of tissue structures and complexes:
- Shattered tissue;
- The anatomical shape of the jaws;
- Bone defects.
In dental implantology:
- Reimplant stabilization;
- Increased alveolar crest;
- Soft tissue buildup;
- Sinus elevation.
Conducting reconstructive plastic surgery for:
- Periodontal disease;
- Periodontitis;
- Osteomyelitis.
Restoration of bone areas after:
- Cystectomy;
- Tooth extraction;
- Injuries;
- Osteomyelitis;
Spongy bone tissue (blocks, cylinders, powder, powder):
- Для замещения дефектов костной ткани при кистах челюстей;
- Для заполнения лунки зуба;
- При синус-лифтинге;
- При аугментации;
- Для увеличения объёма костной массы;
- При вторичной атрофии альвеолярного гребня.
Demineralized bone composite (spongy bone and bone powder):
- For the localized form of periodontitis.
Bicortical and tricortical:
- To restore the upper and lower jaws.
Dura mater:
- For directional regeneration when installing implants;
- Defect cover;
- Schneider membrane protection.
9. Substitution of Dura mater connective tissue complex


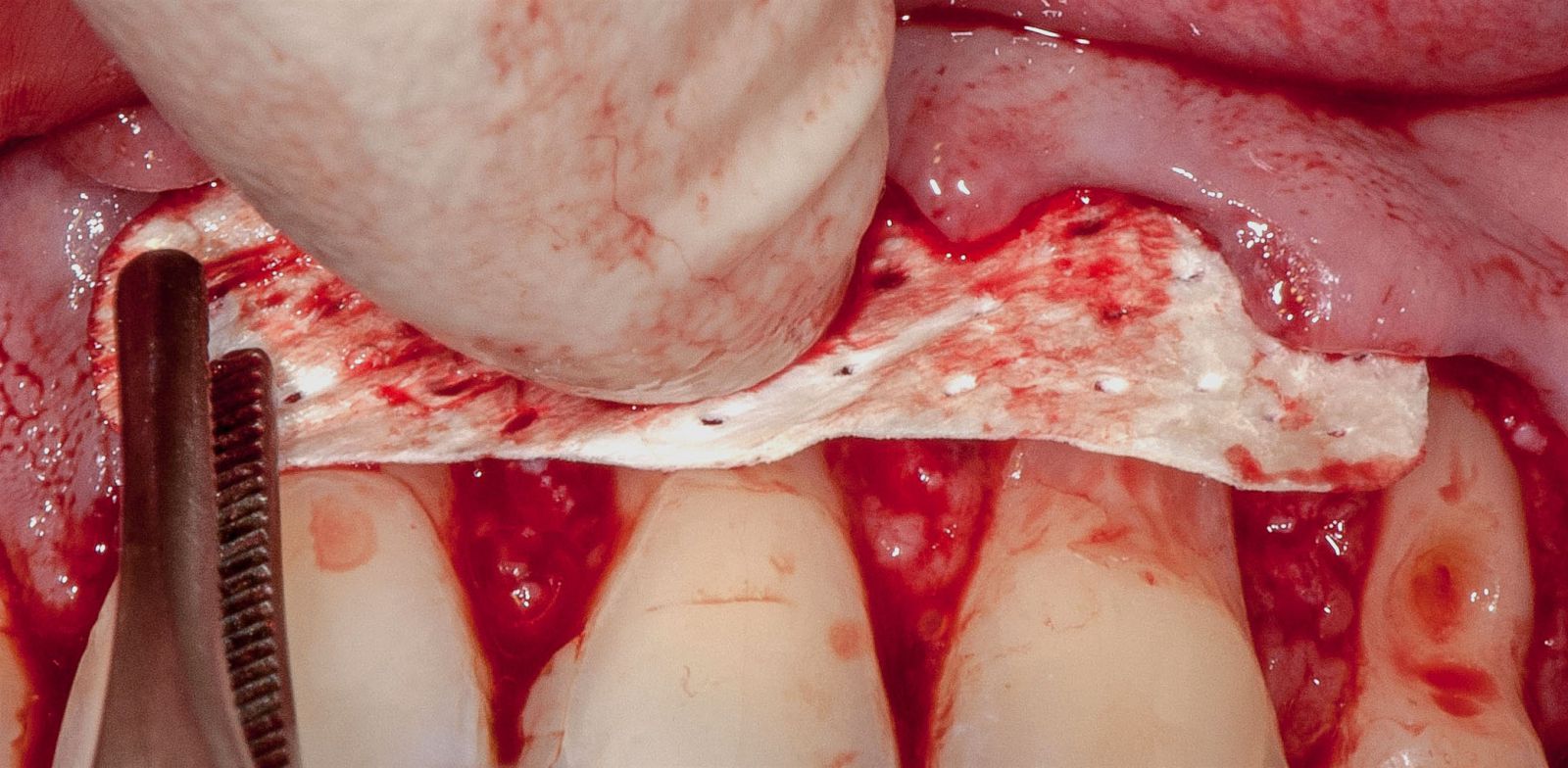
Perforated Collagen membrane (Dura mater) provides an outflow of exudate from the surgical field and carries all the damage factors to trigger reparative and immune processes.It germinates more quickly with blood vessels and is completely replaced in the volume in 100% of cases.
Normally, it is replaced with a cloth in 4 months, even if it is not perforated.
According to the data of histological analysis, after 4 months in this area there is no structurally releasable Dura mater at all, and its entire volume is completely replaced by soft gingival tissues.


According to the dissertation (Omsk, 1980) with the introduction of Dura mater in the bone (under the periosteum in a crushed form), it is completely replaced by bone tissue without a residue.In this case, the formed bone is completely identical to the bone tissue in the adjacent areas.
The process of resorption and replacement of Dura mater is controlled by creating a transport of fluids through the membrane while maintaining its barrier properties.A tool for this is the presence of perforations in the Dura mater with a certain frequency and diameter.
10. Areas of Clinical Use of Lyoplast Bioimplants
The basis of the developed operations with the use of biomaterials "Lyoplast" is based on the principle of individual selection of osteoplastic materials.Anatomical and histological features of the structure of a bone damaged by diseases or injuries, its regenerative potencies, the degree of maturity of the bone tissue from which the graft is made are taken into account.
A complex of therapeutic measures applied before the operation, during its implementation, and in the postoperative period.
These measures are aimed at the maximum elimination of the pathological condition in the bone, both through surgical techniques, and due to physiological factors and mechanical devices.
Combined treatment methods contribute to the elimination of the pathological changes in the bone, the full restoration of its shape, structure and functions.
Application in dentistry and maxillofacial surgery.
1. With periodontal disease:
a) Local form - Demineralized bone composite. (Demineralized spongy bone fragment + Demineralized bone powder). The bone is rebuilt within 2-3 months.
b) Generalized form - demineralized compact bone tissue in combination with demineralized bone powder.
2. To replace the tooth hole and bone defects in the jaw after cystectomy:
Spongy crumb mineral-containing or spongy blocks.
3. For simultaneous and delayed dental implantation:
Spongy crumb mineral-containing and demineralized cortical powder.
Dura mater - as a membrane for directed regeneration.
4. In case of atrophy of the alveolar ridge with adentia:
To restore the shape, volume and height of the alveolar ridge, mineral-containing spongy crumb in combination with MCC powder (mineral component of the bone) or without it.
5. With periimplantitis:
Demineralized bone powder or demineralized spongy crumb mixed with mineralized.
6. To replace jaw fragments:
Right and left halves of the lower jaw, fragments of the ilium (bicortical and tricortical blocks).
7. Sinus lift:
Mineral spongy crumb + MSC + DIPA.
8. In pediatric dentistry with tooth-containing cysts for filling a tooth hole:
Demineralized spongy crumb.
The use of osteoplastic materials helps to restore the destroyed areas of tissue, the anatomical shape of the jaws and provides tooth preservation and compensation for bone defects.